In healthcare, the only constant is change! And we have seen evidence of that continuous change in how ICUs or intensive care units are designed and constructed.
“The hospital is a human invention and can be reinvented at any time.”
Healthcare Futurist Leland R. Kaiser, Ph.D.
These words ring true, as healthcare architecture is a significant part of that change. Over the last few years, we have seen considerable improvements in how ICU setups are planned and executed.
The spark that inspired this focus on ICU design stems from many factors; however, one can’t deny the effect of the COVID pandemic and the way it highlighted the need for more patient-centred care. ICUs are not just limited to single units housing all critical patients. If the facility has independent units for surgery, paediatrics, neonatology, and cardiac diseases, each branch often has its separate ICUs. Let’s look at how the ICU has changed over time to meet the healthcare centres’ requirements.
Types of ICU Designs
1. Combined Critical Care
Rural or regional hospitals must be flexible with how they allot and use beds. So, their ICU area may house a mix of short and medium-term intensive care patients when required. They also accommodate patients from medicine and surgery together in one place to suit a lower nurse-to-patient ratio.
2. The ‘Hot Floor’ model
A hot floor model combines all the various ICUs into one specific location or floor in a hospital. They may house their satellite lab to get access to rapid blood investigations or have their emergency operation theatre, cardiac care unit, and medical imaging devices. The idea is to collate services, avoid duplication of staff and equipment and manage a more efficient deployment of nurses for standardized care. The disadvantage of such a model is that vulnerable patients from different specialties are housed close together and share the services of a common group of nurses and doctors, increasing the risk of cross-contamination and infection outbreaks.
3. Separate ICUs
This model covers a range of specialty ICUs provided as disconnected units in separate locations, with an independent management structure for each team. This is usually possible in larger healthcare centres with high patient loads.
Even though different organizations may opt for different ICU outlines, some elements remain constant and should be kept in mind when designing an intensive care unit. Here are a few to consider.
Essential Elements in ICU Design
Intensive care units are often grouped into different areas based on function. These include:
1. Patient Care Area
a. Electrical Outlets
Electrical Sockets should be accessible from both sides of the patient bed and arranged to provide enough space for multiple devices simultaneously. In addition, 50% of the electrical outlets in the patient room are usually connected to the hospital emergency power system (uninterrupted power supply or UPS) to ensure that the vital life support machines remain functional even during power outages.
Adequate electrical outlets and space should be provided for pumps and IV bags to administer IV fluids and medicines. Most pumps are connected electronically to patient monitoring systems.
b. Vacuum Outlets
Vacuum and compressed air outlets are needed for several bedside procedures:
- Intubation or extubating procedures that need access to oxygen Face and aerosol masks should be accessible from both sides of the bed.
- Endoscopy
- Patients with multiple drains (such as chest tubes and wound drainages).
c. Isolation rooms
With the emergence of highly infectious diseases that spread quickly, especially in healthcare organizations, isolation rooms have become a requirement for ICUs. They are usually built with airlocks, closed rooms that separate two different areas. These airlocks prevent direct airflow between these areas when people come in and out.
The air pressurization systems could differ based on the nature of the infection that needs to be stopped from spreading. On that front, Isolation Rooms can be classified as Positive Isolation Rooms and Negative Isolation Rooms. Find out more about how isolation areas are built in our blog linked here!
Heating, ventilation, and air-conditioning (HVAC) are also necessary for infection control. Maintaining good indoor air quality (IAQ) prevents hospital-acquired infections.
The essential features of a sound HVAC system include:
- Heating and cooling
- Humidifying and dehumidifying to maintain the moisture content of the air
- Filtration to remove dust particles, biological contaminants like bacteria, viruses, and fungi
- Ventilation to facilitate air exchange between outdoor and indoor areas
- Air distribution, which checks the velocity, flow pattern, and direction of movement
d. Access to Clinical Laboratory Services
ICUs should have access to 24-hour clinical laboratory services. These can be provided by a central hospital laboratory or a satellite laboratory within or near the ICU. Satellite labs have essential machines required in emergencies, like blood counts and blood gas analysers.
Some organizations have pneumatic chutes for sample transport to get faster reports.
e. Environment and Fixtures
Clever design can make processes simple for healthcare providers and improve patient care.
- Doors: The door system should be large enough to allow patients’ beds, with their equipment accompanying personnel, to enter. Sliding glass doors with an opening capacity can provide more visibility to the patient and are wider, allowing for easy and rapid transport.
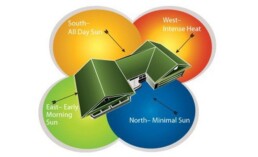
- Windows: Natural light is essential to the well-being of patients and staff. Providing patients with an external view – preferably facing a garden or courtyard – can help relieve anxiety and stress.
- Lights: Indirect and soft light can be used instead of harsh, fluorescent ones to create a soothing environment.
Find out more about how design elements can help with mental health and healing for patients in our blog linked here.
2. Staff Support Area
Healthcare providers must be given the right tools and a supportive environment to deliver their services effectively for patient well-being. The right design and planning can ensure the following:
a. Administrative support:
Check if the computer terminals are well connected to internet services to facilitate a fast and uninterrupted data flow from patient monitoring devices.
b. Communication systems:
The ICU should have in-unit, in-hospital, and out-of-hospital telephone facilities, an intercom system to communicate between the sub-units of the ICU, and an in-unit alarm system.
c. Personnel Support Room:
ICU doctors and nurses need a quiet place to sleep, eat, relax, take care of personal needs and store their belongings. These rooms often contain:
- Sleeping areas
- Toilets and locker rooms
- Telephones or intercom systems
- Comfortable seating area
3. Family Support Area
Visitor waiting areas and counselling rooms are often filled with anxious relatives waiting for news about their loved ones. Empathetic facility design can ensure that their surroundings don’t add to their stress. For example, a warm room with indirect, natural lighting, pleasant artwork, positive distractions, and open windows would be ideal.
“There is no doubt that relatives of ICU patients need a comfortable environment as they go through the roller coaster of emotions that come when a family member is in the ICU. The guiding principle for any architect is to design, keeping the patient and caregivers in mind. The rest will follow.”
Ar, Kshititi Nagarkar, Shree Designs
Shree Designs has had the pleasure of working with the Government of Uttarakhand to assist them in the architectural planning and execution of the ICU at their District Hospital in Pithoragarh, in collaboration with Aarka Consultants. The ICU was planned per NABH norms and covered nearly 2,600 sq. ft. Find out more about this project through this link!
Related Posts
Designing Healthcare Facilities
Building Better Day Surgery Centres
Efficient care, happier patients, and smarter workflows - this is what defines a successful…
Designing Healthcare Facilities,Infographic,Project Management
Designing Healthcare Spaces That Truly Heal
From concept to completion, every medical space we design prioritizes patient flow, staff…
Designing Healthcare Facilities
The Business of Wellness
In the $1.8 trillion wellness industry, first impressions matter. Patients don’t just choose a…
Designing Healthcare Facilities
Efficient Hospital and Clinic Design
India’s emerging cities are growing rapidly, creating an urgent demand for accessible and efficient…
Designing Healthcare Facilities
Creating Calming and Confidential Spaces for Fertility Clinics
As the demand for fertility treatments grows, the architecture of these clinics plays a vital role…
Designing Healthcare Facilities
Designing the Perfect Hospital Pharmacy
Hospital pharmacies are the backbone of seamless patient care. From efficient workflows to secure…
Designing Healthcare Facilities
Preventive Care Facility Design Strategies
With preventive care emerging as the future of healthcare, this post outlines key architectural…
Designing Healthcare Facilities
Thermal Comfort Decoded
Thermal comfort plays a critical role in patient recovery, staff productivity, and overall…
Designing Healthcare Facilities
Building for Tomorrow: The Imperative of Adaptable Healthcare Design
Healthcare facilities need to be as dynamic as the industry itself. Traditional, rigid designs can…
Designing Healthcare Facilities
Designing Single Speciality Healthcare Centres
As single-speciality centres grow, their design needs become more specific, calling for tailored…
Designing Healthcare Facilities
Innovative Design Solutions for Senior Care Facilities
Designing senior-friendly spaces in healthcare facilities is crucial for catering to the evolving…
Designing Healthcare Facilities
Designing a Dental Clinic for Success
Providing quality dental care is not just about the technical elements of the treatment. It's also…
Designing Healthcare Facilities
3 Lessons Learned While Building a Cardiac Cath Lab
Cardiac care design is moving at the sound of a new beat! The number of Cath labs in India has…
Designing Healthcare Facilities
5 Essential Elements of Healthcare Design
Design makes a significant impact on the delivery of care for both healthcare providers and…
Designing Healthcare Facilities
5 Best Ways to Create Healing Spaces for Kids
Designing spaces in healthcare facilities tailor-made for children is a lesson in balance! A…
Designing Healthcare Facilities
Top 5 Trends in Healthcare Design
Design can make all the difference when it comes to improving patient care. From a patient’s point…
Designing Healthcare Facilities
The Architectural Design of Hospital Facilities
Shree Designs designed and executed many efficient and safe healthcare setups in the middle of the…
Designing Healthcare Facilities
Dauntless Designers
Healthcare Radius in its 7th Anniversary Special issue in October 2019, featured a "power list of…
Designing Healthcare Facilities
The changing face of healthcare design
After completing a decade in designing healthcare projects, Kshititi Nagarkar, principal architect,…
Designing Healthcare Facilities
Thumb Rules for Planning and Designing of Hospitals
Traditional rules of thumb in healthcare planning have changed. Once-accepted rules can now be the…