Thermal Comfort Decoded: How Hospitals Keep Patients Safe and Staff Productive
“When we design for healthcare, we’re designing for life. The right balance of temperature, humidity, and airflow doesn’t just support patient recovery—it helps create a sense of safety and well-being, which is essential in a hospital setting,”
Kshititi Nagarkar, lead architect, Shree Designs
In healthcare environments, thermal comfort plays a critical role in patient recovery, staff productivity, and overall operational efficiency. Unlike standard buildings, hospitals face unique challenges in maintaining optimal indoor conditions due to the diverse needs of patients, staff, and medical processes.
By incorporating thermal comfort approaches into hospital design plans, healthcare architects and hospital planners ensure that it becomes an integral part of creating healing spaces.
Whether you’re building a new hospital or enhancing an existing one, prioritizing HVAC innovations in your hospital architecture design and planning is essential for achieving optimal patient recovery and operational efficiency.
Struggling to adapt existing buildings for healthcare? Check out Repurpose and Resuscitate! for tips on adaptive reuse.
Key Elements of Healthcare-Specific Thermal Comfort Systems
Thermal comfort elements are particularly critical when embarking on a hospital planning and designing project, where every detail contributes to comfort, safety, and operational success.
1. Precise Temperature Regulation
Unlike standard buildings, hospitals require precise temperature ranges tailored to patient conditions.
- For instance, elderly patients benefit from warmer environments due to reduced metabolic rates, while infants require stricter temperature controls to prevent hypothermia.
- Specific zones, such as patient rooms, operating theatres, and waiting areas, demand separate temperature settings to ensure comfort and efficiency. This granular control is essential when developing the best small hospital design or large-scale healthcare projects.
Design thinking in healthcare emphasizes patient-centred solutions, and temperature regulation plays a significant role in creating a soothing environment that supports recovery.
2. Humidity Control
Maintaining optimal humidity levels (40-60%) is integral to a hospital design plan, as it prevents respiratory discomfort and reduces the spread of airborne pathogens.
- Burn victims and immunocompromised patients, for instance, require environments with adjustable humidification to avoid dehydration and infection risks.
- In hospital architecture design & planning, advanced humidification systems can be seamlessly integrated into the HVAC infrastructure to cater to these sensitive needs.
Humidity control also aligns with medical furniture design, as moisture-resistant materials are needed in areas prone to fluctuating humidity levels.
3. Zoned Ventilation
Zoned ventilation systems add value to hospital planning and designing, as they manage airflow, prevent cross-contamination, and optimize energy efficiency.
- Dedicated ventilation systems for different areas, such as isolation wards and operating rooms, ensure specific airflow rates based on patient activity and occupancy levels.
- For building a hospital project, incorporating these systems enhances air quality, an essential factor in both patient care and staff well-being.
4. Individual Patient Controls
Bedside controls for temperature and airflow allow patients to adjust their immediate environment, boosting satisfaction and recovery rates. Portable cooling or heating devices for patients with specific needs, such as post-surgical recovery.
5. Advanced Monitoring Systems
Modern HVAC systems in hospitals rely on advanced technologies for continuous monitoring and optimization. Real-time sensors track critical variables like temperature, humidity, and CO₂ levels, ensuring a safe and comfortable environment. AI-driven systems analyze this data to predict and prevent HVAC issues, contributing to operational excellence in hospital planning and designing.
Challenges in Healthcare Thermal Comfort
1. Diverse Occupancy Needs
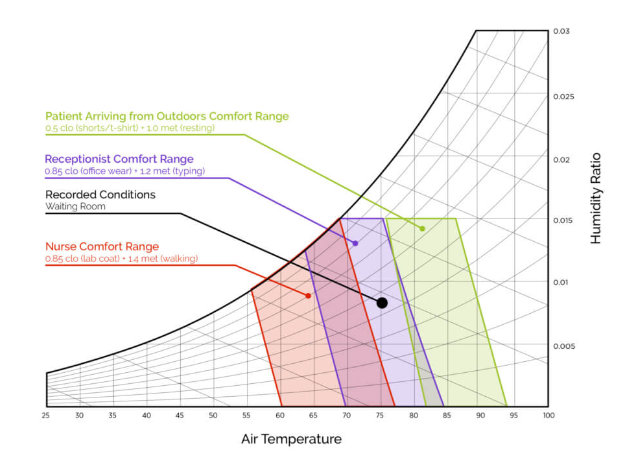
Patients and staff often have conflicting thermal comfort requirements due to differences in activity levels, clothing insulation, and medical equipment. For example, a surgeon wearing insulating garments in an operating room may require cooler temperatures, while a patient undergoing recovery may prefer a warmer environment.
2. Transient Nature of Occupants
Patient turnover and fluctuating occupancy make it difficult to maintain steady-state thermal conditions.
3. Complex Environmental Factors
Healthcare environments are influenced by radiant temperature, air velocity, and humidity, which are not always accounted for in standard thermal comfort models like ASHRAE 55.
4. Energy Efficiency vs. Comfort
Hospitals are energy-intensive, with HVAC systems accounting for significant thermal and electrical energy consumption. Balancing comfort with energy efficiency is a persistent challenge.
Innovative Solutions and Technologies
1. Radiant Heating and Cooling Panels
Evenly distribute heat without creating drafts, making them ideal for patients with limited mobility or burn injuries.
2. Smart Building Integration
HVAC systems linked to centralized building management systems improve energy efficiency and comfort through real-time adjustments.
3. Internet of Things (IoT) Platforms
Low-cost sensor networks measure critical variables like temperature, humidity, and CO₂, feeding data into multidimensional models for rapid decision-making.
4. Personal Cooling Systems
Portable devices that deliver localized cooling or heating for patients and staff with specific needs.
5. Energy-Efficient HVAC Systems
Optimizing HVAC operations can significantly reduce energy costs. For example, intelligent ventilation systems automatically adjust airflows to match room occupancy.
6. Indoor Air Quality (IAQ):
According to the WHO, inadequate IAQ contributes to 99,000 deaths annually. Enhanced filtration systems reduce CO₂, PM2.5, and VOCs, minimizing the risk of respiratory diseases and improving overall health outcomes.
Adapting Thermal Comfort for Healthcare: Addressing Diverse Needs
Designing HVAC systems for hospitals to create optimal thermal comfort demands thoughtful design solutions tailored to varying environmental, patient-specific, and regulatory requirements.
1. Geographic Adaptations: Designing for Extreme Climates
Healthcare design must address the challenges posed by different climates. In cold climates, hospitals often integrate insulated walls, radiant heating systems, and high-efficiency humidifiers to maintain warmth and humidity. These features are crucial in preventing respiratory discomfort and ensuring patients, particularly the elderly, remain comfortable.
Conversely, hospitals in hot climates rely on high-performance cooling systems, reflective coatings, and advanced thermal insulation to combat extreme heat, creating a stable environment for both patients and medical equipment.
2. Addressing the Needs of Specific Patient Groups
Thermal comfort is not a one-size-fits-all solution, especially in healthcare settings where patients may have specific vulnerabilities. Immunocompromised individuals, such as those undergoing chemotherapy or organ transplants, require enhanced filtration systems and HEPA filters to reduce the risk of airborne infections.
Similarly, burn patients benefit from precise humidity control to prevent dehydration and minimize infection risks. Incorporating these tailored solutions into hospital design enhances patient safety and promotes faster recovery.
3. Adhering to ASHRAE Standards for Compliance and Care
Standards like ASHRAE 55 and 170 provide critical guidelines for maintaining temperature, humidity, and ventilation in healthcare settings. However, these standards must be adapted to the unique needs of hospital environments.
For example, while ASHRAE 55 targets general comfort for most building occupants, healthcare facilities require a more nuanced application to address the varying activity levels of medical staff and the specific thermal preferences of patients. Proper implementation ensures a balance between regulatory compliance and personalized care.
Learn how to support healthcare staff with smart layouts in Ergonomics in Healthcare Design.
Conclusion
Thermal comfort in healthcare environments is a multifaceted challenge requiring precise control, advanced technology, and thoughtful design.
“If we get thermal comfort right, we’re not just making people comfortable—we’re actively aiding their recovery,” continues Kshititi.
With continuous advancements in HVAC technology and a focus on sustainable design, the future of thermal comfort in healthcare is both patient-centric and environmentally responsible.
References:
https://www.sciencedirect.com/science/article/abs/pii/S2352710221013218
https://commons.bcit.ca/besys/files/2018/08/Thermal-comfort-health-care.pdf
https://www.sciencedirect.com/science/article/abs/pii/S0360132306002083
https://www.payette.com/conferences/examining-thermal-comfort-for-healthcare/
Related Posts
Designing Healthcare Facilities,Infographic
Blueprint for Healthcare Design
From room dimensions to lighting levels, every detail matters in healthcare design. At Shree…
Designing Healthcare Facilities
Building Better Day Surgery Centres
Efficient care, happier patients, and smarter workflows - this is what defines a successful…
Designing Healthcare Facilities,Infographic,Project Management
Designing Healthcare Spaces That Truly Heal
From concept to completion, every medical space we design prioritizes patient flow, staff…
Designing Healthcare Facilities
The Business of Wellness
In the $1.8 trillion wellness industry, first impressions matter. Patients don’t just choose a…
Designing Healthcare Facilities
Efficient Hospital and Clinic Design
India’s emerging cities are growing rapidly, creating an urgent demand for accessible and efficient…
Designing Healthcare Facilities
Creating Calming and Confidential Spaces for Fertility Clinics
As the demand for fertility treatments grows, the architecture of these clinics plays a vital role…
Designing Healthcare Facilities
Designing the Perfect Hospital Pharmacy
Hospital pharmacies are the backbone of seamless patient care. From efficient workflows to secure…
Designing Healthcare Facilities
Preventive Care Facility Design Strategies
With preventive care emerging as the future of healthcare, this post outlines key architectural…
Designing Healthcare Facilities
Building for Tomorrow: The Imperative of Adaptable Healthcare Design
Healthcare facilities need to be as dynamic as the industry itself. Traditional, rigid designs can…
Designing Healthcare Facilities
Designing Single Speciality Healthcare Centres
As single-speciality centres grow, their design needs become more specific, calling for tailored…
Designing Healthcare Facilities
Innovative Design Solutions for Senior Care Facilities
Designing senior-friendly spaces in healthcare facilities is crucial for catering to the evolving…
Designing Healthcare Facilities
Designing a Dental Clinic for Success
Providing quality dental care is not just about the technical elements of the treatment. It's also…
Designing Healthcare Facilities
3 Essential Design Features for Intensive Care Units
ICUs are not just limited to single units housing all critical patients. If the facility has…
Designing Healthcare Facilities
3 Lessons Learned While Building a Cardiac Cath Lab
Cardiac care design is moving at the sound of a new beat! The number of Cath labs in India has…
Designing Healthcare Facilities
5 Essential Elements of Healthcare Design
Design makes a significant impact on the delivery of care for both healthcare providers and…
Designing Healthcare Facilities
5 Best Ways to Create Healing Spaces for Kids
Designing spaces in healthcare facilities tailor-made for children is a lesson in balance! A…
Designing Healthcare Facilities
Top 5 Trends in Healthcare Design
Design can make all the difference when it comes to improving patient care. From a patient’s point…
Designing Healthcare Facilities
The Architectural Design of Hospital Facilities
Shree Designs designed and executed many efficient and safe healthcare setups in the middle of the…
Designing Healthcare Facilities
Dauntless Designers
Healthcare Radius in its 7th Anniversary Special issue in October 2019, featured a "power list of…
Designing Healthcare Facilities
The changing face of healthcare design
After completing a decade in designing healthcare projects, Kshititi Nagarkar, principal architect,…
Designing Healthcare Facilities
Thumb Rules for Planning and Designing of Hospitals
Traditional rules of thumb in healthcare planning have changed. Once-accepted rules can now be the…